Indiana has submitted a proposal for a share of the federal government’s new $50 billion Rural Health Transformation Program, outlining a five-year plan to bolster struggling hospitals, expand essential services and modernize the state’s fragmented rural health infrastructure.
The proposal, named “
GROW: Cultivating Hoosier Health,” was submitted Nov. 4 to the Centers for Medicare and Medicaid Services (CMS). Funding awards must be issued by
Dec. 31, and money would begin flowing to states in 2026. Indiana is applying for the full $1 billion (over 5 years). Indiana’s application includes 12 initiatives, including physician workforce. It would create a rural GME development plan, 15 new rural residency positions, $10,000 preceptor stipends, rural rotations for medical schools, a preceptor database, paying stipends to recruit and retain physicians in areas such as primary care, pediatrics, OB/GYN and general surgery.
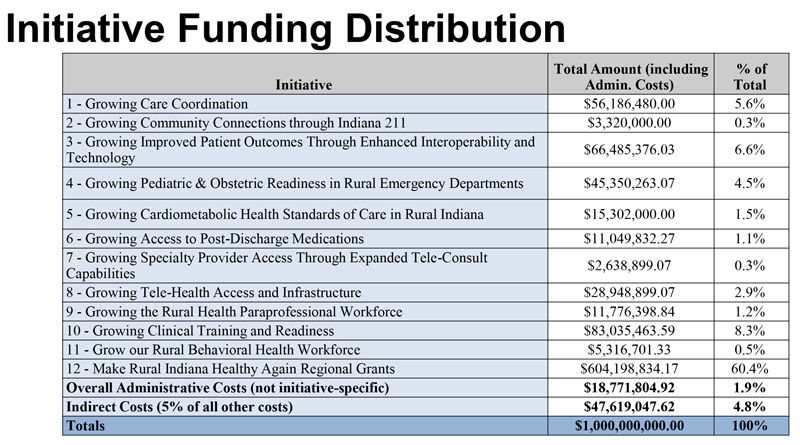 The 12 initiatives in the Indiana Rural Health Transformation grant application are shown with the amount of grant dollars tied to the initiative as well as the proportion of funding overall.
The 12 initiatives in the Indiana Rural Health Transformation grant application are shown with the amount of grant dollars tied to the initiative as well as the proportion of funding overall.
The state emphasized that its Rural Health Transformation proposal was built through “broad, cross-sector collaboration.” The plan is described as a joint effort led by the Indiana Family and Social Services Administration and the Indiana Department of Health, with contributions from rural hospitals, EMS agencies, the Indiana Rural Health Association, tribal groups, managed care organizations and other state and local partners, including ISMA.
Indiana has 64 designated rural counties and 52 rural hospitals, 25% of which have already cut services, according to the Centers for Healthcare Quality and Payment Reform.
If approved, the plan would pump hundreds of millions of dollars into care coordination, technology upgrades, chronic-disease management and emergency readiness beginning in 2026.
Here’s what physicians need to know:
- Faster patient transfers and clearer hospital capacity
A new 24/7 Medical Operations Coordination Center would serve as a statewide hub for patient-transfer requests, hospital capacity reporting and EMS resource alignment.
- Major upgrades to Indiana’s health information exchange
Indiana plans to connect 450 additional rural facilities to the HIE and test predictive analytics and natural-language tools to reduce errors.
- Expanded specialty access and chronic disease management
Eight new rural cardiometabolic care sites would target diabetes, hypertension and obesity through collaborative care teams. The regions are expected to form their own coalitions, identify their own needs, and submit their own project proposals. Each regional committee must include people from certain categories, including a provider representative and a local health department representative.
As of now, there is no public map or county-level breakdown for where the new cardiometabolic centers will go.
- Improved maternal and pediatric emergency readiness
Funding would help hospitals and EMS agencies achieve Pediatric Ready and OB Ready status, designations tied to lower mortality and better emergency response.
Competitive grants could reshape local health systems. The plan’s largest investment, $600 million over five years, would be distributed across eight regional coalitions to support service expansion and care redesign.
- Behavioral health workforce expansion
Indiana seeks to expand rural training tracks and fund stipends tied to working locally for five years.
- Financial stabilization for rural hospitals
Indiana will also study a rural Medicaid payment model to help critical access hospitals and small facilities maintain essential services.
If approved by CMS, funding begins in 2026, with regional grant applications opening in March and awards finalized by October.
Rural physicians, and practices that serve rural populations, should expect more regional collaboration, expanded data-sharing requirements, new referral pathways and technology incentives that could shift daily workflow.