Payer Coverage of COVID-19 and Telehealth Visits
By Carol Hoppe, CPC, CCS-P, CPC-I
MedLucid Solutions
NOTE: The information provided here is the most currently available as of March 20. It is changing constantly. If you have questions not addressed in this document or the references provided, please email Carol Hoppe at
carol@medlucidsolutions.com with COVID-19 in the subject line and we will attempt to find further answers for you or direct you to appropriate resources.
I wanted to provide the latest updates with regards to payer requirements based on the most commonly asked questions coming my way.
I'm also attaching a copy of the screen shots from this morning's Indiana Medicaid teleconference that gives additional information.
The most common questions being asked this week are:
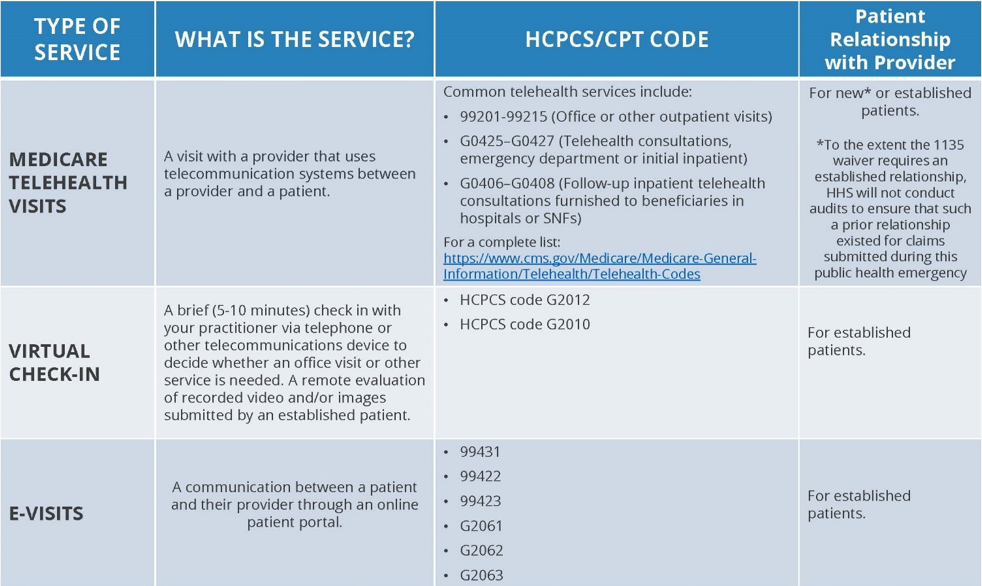
- What is the difference between telephone calls, audio-video conferencing and eVisits and Virtual Check-Ins?
o To bill 99201-99215 via telehealth, you must see the patient using an audio-video method like Skype, Google Hangout, Facetime or doxy.me (reimbursed by most payers at your regular fee schedule rates)
o For telephone-only services, use G2012 for Medicare virtual check-in visits of 5 to 10 minutes (Indiana Medicare reimbursement is $13.92); some commercial payers will reimburse for 99441-99443
o eVisits via online patient portals or email are considered asynchronous and are covered by some payers with codes 99421-99423 or G2061-G2063
- Can we see new patients via telehealth or just established patients?
o This varies by payer. Many payers are allowing for new patient visits; see the updated spreadsheet for those that have indicated 99201-99215 are covered. CMS indicated that the OIG would not audit for an established patient relationship during the government's 1137 waiver period. Some commercial payers are not listing specific codes and I have removed them from my spreadsheet but provided links to their COVID-19 updates. I think we will continue to see changes over time, but I can't give specific guidance that is not clear from those payers.
- What modifiers and place of service codes do I use?
o This varies by payer. See spreadsheet for payer specific guidance.
- What documentation should be included in telehealth visits?
o See attached spreadsheet with recommended documentation based on various payer requests.
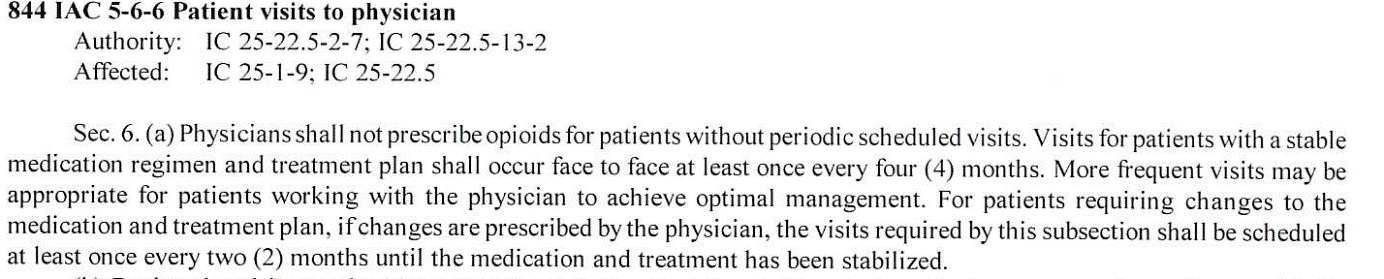
- Can I prescribe opioids for patients seen via telehealth?
o There is still some confusion on this for Indiana providers. The FSSA issued BT202022 stating:
"...to further clarify, Indiana Code does allow a provider to use telemedicine to prescribe a controlled substance to a patient who has not been previously examined. Opioids, however, cannot be prescribed via telemedicine, except in cases in which the opioid is a partial agonist (such as buprenorphine) and is being used to treat or manage opioid dependence."
We are seeking further explanation on what this means exactly since Indiana State law allows patients who are stable without medication changes to be seen face-to-face every four months.
 FinalRule102516-PDF
FinalRule102516-PDF
While the DEA has allowed patients to be seen for controlled substances via telemedicine during the pandemic, practitioners must also act in accordance with applicable Federal and State law.
TELEHEALTH VIA AUDIO-VIDEO TECHNOLOGY
Using
doxy.me is my best recommendation if you have not started using any other audio-video technology. It is extremely easy to use, has a free basic version or you can pay $35.00 per month per provider for additional features such as texting patients with a link to the provider at their scheduled appointment time. Check it out by entering
doxy.me in any internet browser and click Get Started for Free. Select I'm a Provider or I'm a Patient. It's that easy to connect in a provider Virtual Waiting Room by providing patients with a link to the provider's virtual waiting room. Patients and providers can use any smartphone, iPad, laptop or computer to access the Virtual Waiting Room via
doxy.me. [I have no financial interest in this product; I've just seen and heard lots of great feedback.]
While many older patients do not have internet access or data plans on their cell phones, you should encourage them to get with a neighbor or family member who can help them access this functionality. It is extremely beneficial for patients and providers to interact via video conferencing for the best telehealth experience. Indiana Medicaid patients are being given additional phone and data minutes to be able to interact with providers via telehealth.
Indiana Medicaid updates its telehealth guidance; Anthem clarifies policy
By Carol Hoppe, CPC, CCS-P, CPC-I
MedLucid Solutions
NOTE: The information provided here is the most currently available as of March 20. It is changing constantly. If you have questions not addressed in this document or the references provided, please email Carol Hoppe at
carol@medlucidsolutions.com with COVID-19 in the subject line and we will attempt to find further answers for you or direct you to appropriate resources.
On Friday, March 20, the IHCP came out with an update that included important changes in the IN Medicaid section of the Telehealth Coding Options spreadsheet:
- Must use modifier GT for telehealth visits
- DO NOT use POS 02 or 95, or your claims will deny
- Read the complete IHCP bulletin here.
Also, Anthem sent me the following answer this morning:
With the eUpdate that was posted to the Anthem website yesterday, correct that it doesn’t indicate any CPT/HCPCS codes [for telephone codes specifically]. Anthem does not advise providers what codes to bill with, therefore, you would bill for with the appropriate codes based on the services rendered.
Additionally, we have had an Anthem reimbursement Telehealth policy posted to our website that you can review, as well. I have included the link. https://www.anthem.com/docs/public/inline/C-08002.pdf.
The latest updates are highlighted in yellow on the spreadsheet at the link above. ISMA will continue to keep you updated on developments related to COVID-19.
Payer Coverage of COVID-19 and Telehealth Visits
By Carol Hoppe, CPC, CCS-P, CPC-I
MedLucid Solutions
NOTE: The information provided here is the most currently available at the time of publication. It is changing constantly and may have changed by the time you read this. If you have questions not addressed in this document or the references provided, please email Carol Hoppe at
carol@medlucidsolutions.com with COVID-19 in the Subject Line and we will attempt to find further answers for you or direct you to appropriate resources.
Telehealth and Other Technology Services during COVID-19
As of Tuesday, all telehealth services are paid by Medicare under the Physician Fee Schedule at the same amount as in-person services. The Originating Site requirements are waived at least during the COVD-19 emergency. Services listed in Appendix P of the CPT® Code book or on the Medicare telehealth code list can all be provided with patients at home Providers must use an interactive audio and video telecommunications system that permits real-time communication between the distant site (the provider) and the patient at home. “As part of this announcement, patients will now be able to access their doctors using a wider range of communication tools including telephones that have audio and video capabilities, making it easier for beneficiaries and doctors to connect.”
Medicare coinsurance and deductible amounts still apply for these services. However, the Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs.
To the extent the 1135 waiver for COVID-19 requires an established patient relationship, HHS will not conduct audits to ensure that such a prior relationship existed for claims submitted during this public health emergency.
MEDICARE already allows for patients to communicate with their doctors or certain other practitioners for “virtual check-ins” without going to the doctor’s office. These brief, virtual check-in services are for:
- Established patients who have a relationship with a physician or certain practitioners;
- Communication is not related to a medical visit within the previous 7 days and does not lead to a medical visit within the next 24 hours (or soonest appointment available);
- The patient must verbally consent to using virtual check-ins and consent must be documented in the medical record prior to the patient using the service; and
- The Medicare coinsurance and deductible would apply to these services.
Use HCPCS code G2012 for “virtual check-in” when doctors and certain practitioners personally provide these virtual check-in services via telephone.
Use HCPCS code G2010 for “Remote evaluation of recorded video and/or images submitted by an established patient (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment”.
Medicare also pays for patients to communicate with their doctors using online patient portals. The individual communications, like the virtual check ins, must be initiated by the patient; however, practitioners may educate beneficiaries on the availability of this kind of service prior to patient initiation.
- Communications can occur over a 7-day period
- Services may be billed using the following CPT® and HCPCS codes
o G2061 – Qualified nonphysician health care professional online assessment, for an established patient, up to 7 days, cumulative time during the 7 days; 5 to 10 minutes
o G2062 – 11 to 20 minutes
o G2063 – 21 or more minutes
- The Medicare coinsurance and deductible would apply to these services.
Summary of Medicare Telemedicine Services
MEDICARE TELEMEDICINE HEALTH CARE PROVIDER FACT SHEET Mar 17, 2020
MEDICARE ADVANTAGE
Medicare Advantage plans may already provide benefits to their members for telehealth visits, including services when the beneficiary is in a variety of locations including their home.
VACCINE
Once a vaccine is available, all Medicare Part D plans will be required to cover the vaccine.
OTHER PAYERS
Most of the other payers, including Indiana Medicaid, have adopted similar telehealth policies allowing patients to be seen for regular visits using CPT® codes found in Appendix P of the CPT® manual. According to Dr. Ann Zerr, IN Medicaid Medical Director, “The [IN Medicaid] telemedicine policy is being updated to expand some services as a result of the governor’s emergency declaration.”
These are subject to change at any time, so keep an eye out for updates as they become available. Please see the attached spreadsheets.
DIAGNOSTIC TESTING / Looking for Consistent Reporting Across the Country
CMS has created two new HCPCS codes for testing patients for Coronavirus (COVID-19) – HCPCS code U0001 for the Centers for Disease Control and Prevention (CDC) “2019 Novel Coronavirus Real Time RT-PCR Diagnostic Test Panel” and U0002 for “2019-nCoV Coronavirus, SARS-CoV-2/2019-nCoV (COVID-19) using any technique, multiple types or subtypes (includes all targets)”. Medicare and many other payers have adopted these new codes for such tests. The codes have two different reimbursement rates, with the U0001 paying more than the U0002. Medicare will be able to accept these codes on April 1, 2020 for dates of service on or after February 4, 2020.
The American Medical Association (AMA) has issued a new CPT® code 87635 for Infectious agent detection by nucleic acid (DNA or RNA); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]), amplified probe technique. This code is effective immediately and will appear in the 2021 CPT® Code book. The reimbursement for this code should be based off the higher reimbursement rate, so providers are encouraged to use this code for all payers except Medicare.
Diagnosis Coding Tips
To be a covered COVID-19 service, payers are looking for these diagnosis codes for suspected exposure and confirmed exposure:
Z03.818, Encounter for observation for suspected exposure to other biological agents ruled out.
Z20.828, Contact with and (suspected) exposure to other viral communicable diseases.
If COVID-19 is documented as being associated with other respiratory conditions, such as pneumonia or respiratory distress, use B97.29 Other coronavirus as the cause of diseases classified elsewhere, as a secondary code.
For signs and symptoms not yet diagnoses, use
R05
Cough
R06.02
Shortness of breath
R50.9
Fever, unspecified
Diagnosis code B34.2, Coronavirus infection, unspecified, is not appropriate for COVID-19, because the cases have universally been respiratory in nature, so the site would not be “unspecified.”
If the provider documents “suspected”, “possible” or “probable” COVID-19, do not assign code B97.29. Assign a code(s) explaining the reason for encounter (such as fever or Z20.828).
MODIFIERS AND PLACE OF SERVICE CODES
GQ
Services delivered via asynchronous telecommunications system
GT
Face-to-face encounter utilizing interactive audio-visual communication technology
95
Synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system. Modifier 95 is only for codes that are listed in Appendix P of the CPT® manual.
POS 2
Telehealth services
ADDITIONAL REFERENCES
Current Procedural Terminology (CPT®) copyright 2019 by the American Medical Association. All rights reserved.
https://seekingalpha.com/pr/17802516-anthem-s-affiliated-health-plans-waive-member-costs-for-covidminus-19-testing-while
https://www.ahip.org/health-insurance-providers-respond-to-coronavirus-covid-19/
https://www.cms.gov/files/document/03052020-medicare-covid-19-fact-sheet.pdf
https://www.cms.gov/files/document/covid19-emergency-declaration-health-care-providers-fact-sheet.pdf
https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes
https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/TelehealthSrvcsfctsht.pdf
https://www.in.gov/coronavirus/files/IDOI%203.14.20.pdf
https://www.in.gov/medicaid/files/telemedicine%20and%20telehealth%20services.pdf
https://www.uhcprovider.com/content/provider/en/viewer.html?file=https%3A%2F%2Fwww.uhcprovider.com%2Fcontent%2Fdam%2Fprovider%2Fdocs%2Fpublic%2Fpolicies%2Fcomm-reimbursement%2FCOMM-Telehealth-and-Telemedicine-Policy.pdf
https://www.uhcprovider.com/en/resource-library/news/provider-telehealth-policies.html